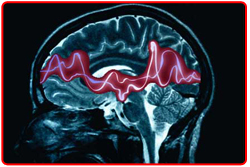
Epilepsy is a common chronic neurological disorder that is characterized by recurrent unprovoked seizures. These seizures are transient signs and/or symptoms due to abnormal, excessive or synchronous neuronal activity in the brain. About 50 million people worldwide have epilepsy at any one time. Epilepsy is usually controlled, but not cured, with medication, although surgery may be considered in difficult cases. Epilepsy should not be understood as a single disorder, but rather as a group of syndromes with vastly divergent symptoms but all involving episodic abnormal electrical activity in the brain.
|
|
 |
 |
|
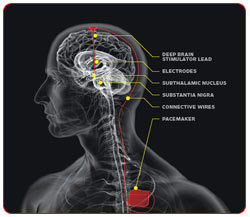
In the majority of patients with epilepsy, seizures can be well controlled with appropriate medication. However, current estimates indicate that 20 - 30% of patients with epilepsy are refractory to all forms of medical therapy. These medically intractable patients are candidates for surgical treatment in an attempt to achieve better seizure control. Another group of patients who might benefit are those whose seizures may be relatively well controlled but who have certain characteristic presentations or lesions that strongly suggest surgical intervention might be curative. Clinical data suggests that continued medical therapy after failure to control seizures with aggressive trials of antiepileptic drugs (AEDs) is not optimal treatment of certain forms of epilepsy. In addition, surgery yields a better quality of life and reduced depression and anxiety as soon as 3 months after surgery compared with continued medical therapy. This improved quality of life is specifically related to the occurrence of complete seizure freedom . |
 |
 |
 |
| Diagnosing Epilepsy |
 |
Diagnosing epilepsy is a multi-step process, usually involving the following evaluations : |
 |
| Confirmation through patient history, neurological exam, and supporting blood and other clinical tests that the patient has epileptic seizures and not some other type of episode such as fainting, breath-holding (in children), transient ischemic attacks, hypoglycemia, or non-epileptic seizures. |
 |
| Identification of the type of seizure involved. |
 |
| Determination of whether the seizure disorder falls within a recognized syndrome. |
 |
 |
 |
| Diagnostic Methods and Tools |
 |
 |
 |
The doctor's main tool in diagnosing epilepsy is a careful medical history with as much information as possible about what the seizures looked like and what happened just before they began. The doctor will also perform a thorough physical examination, especially of the nervous system, as well as analysis of blood and other bodily fluids.
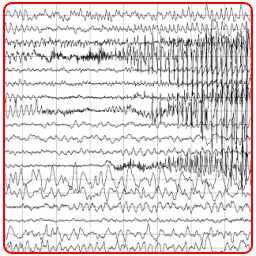
A second battery of diagnostic tools include an electroencephalograph (EEG). This is a machine that records brain waves picked up by tiny wires tapedto the head.
Electrical signals from brain cells are recorded as wavy lines by the machine. Brain waves during or between seizures may show special patterns which help the doctor decide whether or not someone has epilepsy.
|
|
|
| Imaging methods such as CT (computerized tomography) or MRI (magnetic resonance imaging) scans may be used to search for any growths, scars, or other physical conditions in the brain that may be causing the seizures. In a few research centers, Positron emission tomography (PET) imaging is used to identify areas of the brain which are producing seizures. |
 |
 |
 |
| The Decision to Treat |
 |
The doctor's main tool in diagnosing epilepsy is a careful medical history with as much information as possible about what the seizures looked like and what happened just before they began. The doctor will also perform a thorough physical examination, especially of the nervous system, as well as analysis of blood and other bodily fluids. |
|
 |
 |
|
 |
 |
 |
 The Treatment Decision
The Treatment Decision |
 |
 'The decision to treat is highly individualized, weighing the risks of treatment against the risks of seizures’
'The decision to treat is highly individualized, weighing the risks of treatment against the risks of seizures’
 When a child or adult experiences a single seizure, or appears at the doctor’s office with a history of questionable events that may or may not have been seizures, the first issue is to determine what happened, whether a seizure actually took place, of what type and duration it was, the possible cause, and the future prognosis. When a child or adult experiences a single seizure, or appears at the doctor’s office with a history of questionable events that may or may not have been seizures, the first issue is to determine what happened, whether a seizure actually took place, of what type and duration it was, the possible cause, and the future prognosis.
Once this information is gathered, the next question is whether to treat the underlying condition (if one has been identified and if it is treatable), or whether to treat the symptoms by prescribing antiepileptic (or seizure-preventing) drugs.
Unless the EEG is clearly abnormal, thus increasing the likelihood of subsequent seizures, physicians tend to wait until a second or even third seizure occurs before beginning antiepileptic medication. They do so because studies show that an otherwise normal child who has had a single seizure has a relatively low (15 percent) risk of a second one. Once the second has occurred, the risk of subsequent seizures is substantially increased.On the other hand, the risk of another seizure for a child who is neurologically abnormal, or whose EEG is abnormal, may be as high as 50 to 60 percent.
In determining whether to treat, physicians consider the risk-benefit ratio, which varies according to the age of the patient and his or her activity level. Waiting to see whether another generalized tonic-clonic seizure occurs is less risky for a child living in a sheltered home environment than it is for a salesman who lives most of his life driving a car, or an elderly person with brittle bones. On the other hand, antiepileptic drugs have side effects which, while generally mild, can in some cases include liver damage and potentially fatal rashes and blood disorders. Thus the decision to treat becomes a highly individualized one in which the risks of the treatment are weighed against the risks of the seizures. |
 |
 |
 |
 |
| Factors Influencing Decision to Treat |
 |
 |
Abnormal EEG |
 |
Previous Seizure |
 |
Person Drives |
 |
Other Neurological Impairment |
 |
Elderly |
|
| |
| Factors Influencing Decision Not to Treat |
| |
 |
 |
Single Seizure |
 |
Neurologically Normal |
 |
Young Age |
 |
Side Effects |
|
|
 |
|
 |
 |
 |
|
|